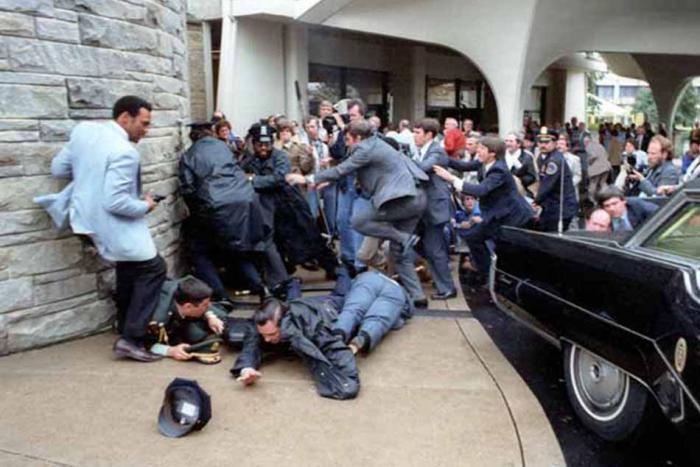
In 2007, Laura shuffled through the sterile hallways of a San Antonio burn unit looking for her son, Jon. She’d received a phone call saying Jon had gotten blown up, and at first Laura thought this meant exactly what it sounded like: that Jon was dead. She didn’t know the lingo yet.
So Laura flew from Boston and found Jon in a back room of the unit, mummified in gauze and pigskin. His limbs were separated by some kind of special chair and his face was splinted with a mask. Laura had read about the mask online. Without it, scorched features morph through recovery and take on knotty profiles. It was there to help Jon’s face retain its shape while what remained of it healed. Jon would be burned beyond recognition, Laura thought numbly, but if the splint mask did its job, he would at least look like a human.
She had learned about the pigskin online, too. She reminded herself that it might be corpse skin, not pig skin. In some instances so much of a patient’s body has been burned that not enough skin remains to graft with, and so human skin must be generated in a lab. Meanwhile, wounds are covered with a pig’s or a cadaver’s.
“Wounded Warriors,” Laura said, repeating the phrase to herself over and over. This, too, she had learned during her research: the institutionalized term for people like her son was not “injured veterans.” Downstairs at the desk, she’d called her son a patient, and had been told by a well-intentioned but stern administrator that the service members preferred, “Wounded Warriors.” That was the lingo, and Laura didn’t want to get it wrong.
“Wounded Warriors,” she whispered again. She stared hazily through the window of her son’s room and felt her stomach twist sharply to one side.
It wasn’t him.
“What?” Laura asked.
“I said, that’s not Jon,” the nurse repeated softly.
“This one’s George,” she continued, pulling gingerly on Laura, “and he’s having a bad day so let’s leave him be. Jon’s in his room. Come on.”
Laura allowed herself to be led like a sleepy child, and walked down the hall and through a sterile antechamber to find her son laid out, his face shiny from some kind of ointment. His grafted leg lay open, peeled underneath a heat lamp. It looked like a hamburger, Laura thought—but after seeing the mummy and all that pigskin, Jon’s injuries seemed like nothing. They seemed like a miracle.
“Where the hell have you been?” he asked.
*
Skin grafts prickle in the sunlight even after healing, making San Antonio, Texas, a painful place for people who have caught on fire. Yet this is the site of Brooke Army Medical Center (BAMC), one of the premier burn units in the United States, the Center for the Intrepid (CFI), a cylindrical building next door to BAMC where stabilized patients go to rehabilitate, and the Warrior and Family Support Center.
Prior to the Vietnam War, losing two legs during combat often meant dying in the dirt. During Vietnam, improvements in battlefield medicine led to droves of traumatized amputees returning home. And thanks to further advancements during the Iraq and Afghanistan conflicts, more wounded make it home alive these days than ever before. Rangers on patrol get blown up and yanked apart, but contraptions like the Kevlar vest keep their internal organs intact. Some survivors fly home as torsos, with beating hearts and functioning livers but without limbs or faces to speak of. Now that bodies are surviving such devastating damage, the onus is on places like CFI to tackle questions such as, “How does a brain damaged quadruple amputee with 80-percent burns and state-of-the-art robotic limbs re-learn how to wipe himself?”
In 2013 alone, there were over 42,000 appointments at CFI.
CFI is a good place to get new limbs. The hands in particular look so lifelike that seeing them stacked ceiling-high in the prosthetics lab (a sort of Santa’s workshop for manmade body parts) prompts an instinctive shudder; the calibre of craftsmanship is so high that it’s easy to mistake them for real, disembodied limbs.
Before progressing to CFI, however, burn patients must be stabilized. Fire can ignite anything, even muscle and bone. The shiny, scarred limbs of survivors often appear smaller than they should, because destroyed tissue has been removed to avoid infection. Excision is complete when a doctor’s scalpel touches healthy tissue, which is vibrant in comparison to what must be carved out. Dead tissue is grey and mottled, and cutting into it releases nothing except gooey pus and stench, whereas healthy tissue bleeds. So you dig until it bleeds.
Following excision, surgeons harvest healthy tissue to cover the open wound. For this they take an instrument resembling a cheese slicer and drag it over skin, covering a wide swath (usually the thigh) to produce flat bands of flesh. They put those through a machine that is sort of like a pasta maker, which splices skin into netting. Mesh maximizes coverage, allowing a finite amount of skin to cover a larger area. Staple that netting to the edges of the wound, and stick the grafted body part under a heat lamp to keep it dry.
Wound care follows, which is not as easy as squeezing on Neosporin. Many of these wounds are caused by Improvised Explosive Devices (IEDs), which are typically packed with projectiles such as nails, steel pellets, screws, and nuts, or noxious chemicals designed to spread as shrapnel. IEDs are typically used as roadside bombs, and are known as “dirty bombs.” Usually this means the bombs contain biohazardous material. But Dr. Booker King, the director of BAMC, says that the term “dirty bombs” is used among doctors to allude to the fact that these bombs are disgusting. Whether this is because they’re cobbled together with rusty, re-used parts that, when lodged inside a wound, precipitate septicity, or because insurgents are purposely coating the bombs with mysterious pathogenic material, doctors at BAMC can’t (or won’t) say. They do, however, admit that infection during wound care kills many. Whether on the battlefield or at BAMC, burn patients are always at risk for sepsis.
Since IEDs are routinely delivered via human carriers, there have been a small number of suicide bombings to date where human remains shrapnel not only caused grievous injury but also blood-borne illness. In other words, if the individual wearing the explosive device was hepatitis B- or HIV-positive, explosion casualties must be appropriately treated for pathogen exposure. During wound cleaning, doctors not only remove metal fragments and the patient’s own destroyed tissue, but may also dislodge body parts belonging to other humans.
That’s it. Excision, grafting, wound care. Voila: fixed.
Not really. It isn't easy to put a person back together. You need surgeons, sculptors, scientists, psychologists, and healthy tissue. And still, it doesn't always work.